Dry Eyes
Dry Eye Syndrome, also known as ocular surface disease, keratoconjunctivitis sicca (KCS) or keratitis sicca; is a multifactorial disease of the tears and the ocular surface that results in discomfort, visual disturbance and tear film instability with potential damage to the ocular surface. Dry Eye Syndrome is typically characterized by symptoms of dry, gritty eyes, stinging, burning, itching and overall discomfort.
Nature provided our eyes with tears to wash away irritants, lubricate the lids, and to keep our cornea moist. Sometimes, the lacrimal gland or associated glands near the eye don’t produce enough tears, or dysfunction of the meibomian glands reduces oil output, leading to excessive evaporation of the tears resulting in Dry Eye Syndrome. Excessive dry eyes, if left untreated, can harm your eyes by damaging tissue and possibly scarring the cornea of your eye, impairing vision.
What’s in a Tear?
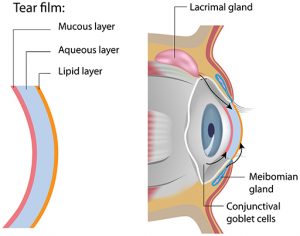
Tears consist of three essential components:
- The outer, oily lipid component
- The middle, watery, lacrimal component
- The innermost component, consisting of mucous or mucin
Each component of the tear film serves an important purpose. For example, tear lipids prevent evaporation and increase lubrication, while mucins help anchor the tears to the ocular surface.
Each tear component is produced by a different gland:
- The outer oily component is produced by meibomian glands in the eyelids.
- The watery component is produced by lacrimal glands located above the outer corner of the eyes.
- The inner mucoid component is produced by goblet cells in the conjunctiva.
A problem with any of those sources can result in tear instability and dry eyes.
Tremendous research and development has occurred and is still being developed because Dry Eyes has been an increasing problem for many people. There have been some great advances in the last few years.
WHAT CAUSES DRY EYE:
- Part of the natural aging process in both men and Women; however, dry eye is typically more prevalent among women (especially during menopause, due to fluctuating hormones);
- A side effect of many medications, including: antihistamines, antidepressants, some blood pressure medications, Parkinson’s medications and oral contraceptives;
- Air conditioning or a dry heating system at your home or office;
- Residing in a dry, dusty or windy climate;
- Insufficient blinking as a result of excess screen time (computers and handheld devices);
- A symptom of a systemic disease, such as: lupus, rheumatoid arthritis, ocular rosacea, or Sjogren’s Syndrome;
- Smoking can increase your risk of dry eyes;
- Injury to the cornea or eye lids;
- Long-term contact lens wear.
DIAGNOSING DRY EYES:
Before any treatment protocol can be established a comprehensive dry eye assessment will be required. An optometrist can detect dry eyes using several different dry eye tests that work collaboratively to evaluate the quality and amount of tears.
- Dry Eye questionnaires – Completed by the patient as a reference for how severe dry eye symptoms are perceived, what medications are taken and an autoimmune assessment profile.
- Phenol Thread / Schirmers – Tests for aqueous deficiency.
- Meibomian Gland Manual Expression – This shows us whether your mebomian glands can secrete lipid under normal blinking.
- Tear Break-up Time (TBUT) – The time required for dry spots to appear on the corneal surface after blinking. A method of determining the stability of the tear film and checking for evaporative dry eye.
- LipiScan – LipiScan was the first dedicated meibomian gland imager. Designed to make high-definition meibography accessible for any practice. It captures high-definition images of gland structure using the Dynamic Meibomian Imaging (DMI) mode in about 60 seconds.
- TearLab – The TearLab Osmolarity System is intended to measure the osmolarity of human tears. Hyperosmolarity is a primary marker of tear film integrity. When the quantity or quality of secreted tears is compromised, increased rates of evaporation lead to a more concentrated tear film (increased osmolarity) that places stress on the corneal epithelium and conjunctiva.
- InflammaDry – InflammaDry® is the first and only, rapid, in-office test that detects MMP-9, an inflammatory marker that is consistently elevated in the tears of patients with dry eye disease. InflammaDry® accurately identifies elevated levels of MMP-9 protein in tear fluid samples taken from the inside lining of the lower eyelid, the palpebral conjunctiva.
HOME RELIEF FOR DRY EYE:
- Over-the-counter artificial tears;
- Omega 3 supplements to help increase the oil production of the tear glands;
- Install a humidifier in dry areas of your home or office;
- Drink water – at least 8 glasses a day, if possible;
- Reduce caffeine intake;
- Reduce alcohol consumption;
- Quit Smoking;
- Your eyes need a break. Limit contact lens wear time once in a while;
- Reduce computer and handheld device screen time, remember to blink!
POSSIBLE TREATMENT OPTIONS:
Artificial Tears – Artificial tears can be prescribed. These are lubricating solutions that closely resemble normal tears. However, for maximal relief, these typically need to be used several times in a day.
Night-time Ointments – If symptoms are severe or you do not close your eyes completely while sleeping, these ointments may help to keep your eyes lubricated at night.
Restasis – RESTASIS® (Cyclosporine Ophthalmic Emulsion) 0.05% is the only prescription eye drop that helps increase your eyes’ natural ability to produce tears, which may be reduced by inflammation due to Chronic Dry Eye disease.
Xiidra – Xiidra® (lifitegrast ophthalmic solution) 5% is indicated for the treatment of signs and symptoms of dry eye disease (DED).
TrueTear – Allergan TrueTear® is a drop-free, drug-free FDA-approved device to increase production of real tears. TrueTear® causes your eyes to produce their own natural tears using tiny pulses of energy. These pulses activate a natural response through a clever technology called neurostimulation.
Punctal Plugs – An alternative to using artificial tears are punctal plugs. These are small silicone plugs that are inserted into an eye’s tear ducts to slow drainage and loss of tears by blocking the tear ducts. This keeps the remaining tears on the eye providing more moisture and comfort. Punctal plugs are a permanent solution but can be removed if necessary. Often times, by plugging up the tear ducts with punctal plugs, artificial tears can be completely eliminated.
LipiFlow – LipiFlow® is a new procedure designed to treat the root cause of Evaporative Dry Eye, blocked Meibomian glands. Opening and clearing these blocked glands can allow them to resume natural production of lipids (oils) needed for a healthy tear film. The treatment is performed in a doctor’s office — and in some cases, on the same day as your evaluation. If this treatment option is deemed appropriate, our office will be happy to refer you out to a trusted specialist.
Amniotic Membrane – In many patients the healing process results in the formation of corneal scar tissue. The amniotic membrane allows for a regulated and regenerative healing process.
Contact Info
- 9671 N Nevada Street
- Suite 210
- Spokane, WA, 99218
Phone: 509-468-2020
Fax: 509-468-3272
[email protected]
Hours
- Monday
- 8:30am - 5:30pm
- Tuesday
- 8:30am - 5:30pm
- Wednesday
- 8:30am - 5:30pm
- Thursday
- 8:30am - 5:30pm
- Friday
- 8:30am - 1:00pm
- Saturday
- Closed
- Sunday
- Closed
Learn more about EyeDentity Eyecare + Eyewear or schedule a time to see one of our doctors today!
